
Pediatric NeuroNews
October 22, 2013
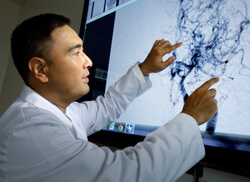
Moyamoya can be a tough disease to diagnose, says pediatric neurosurgeon Edward Ahn. Though it tends to cluster in certain geographic regions, such as East Asia, worldwide incidence is exceedingly low, on the order of about one in a million. Complicating diagnosis is the fact that strokes—typically the first outward manifestation of the disease—are also rare in children.
As a result, says Ahn, “many practitioners might initially misinterpret what’s happening and miss the opportunity for a faster diagnosis and treatment.”
Moyamoya is usually diagnosed from the characteristic appearance of affected blood vessels on MRI and cerebral angiogram. For patients whose disease is in the early stages, therapy often centers on aspirin or other anticlotting agents. But as the disease progresses, surgery eventually becomes the only way to stem the recurrent strokes this disease causes.
Ahn and his Johns Hopkins colleagues tailor their operations depending on the specifics of each case. The option they most commonly choose involves taking a blood vessel not affected by the disease—usually the superficial temporal artery—and redirecting it on top of the brain. Even when they do not connect it directly to affected vessels, the brain grows its own new vessels to tap into the new blood source.
“In cases where the disease has progressed far enough,” Ahn explains, “the brain responds to a new blood supply very well. It’s starving for new blood. If we supply that, the brain readily picks it up.”
For children who continue to have strokes even after these treatments, Ahn and his colleagues perform a procedure recently developed in Korea. Rather than transplanting blood vessels, the neurosurgeons transplant a layer from the scalp directly onto the brain, encouraging the growth of new blood vessels with this tissue.
Ahn estimates that he and his colleagues perform an average of 10 operations for children with moyamoya each year, making Johns Hopkins one of the most active medical centers for treating this disease. In most cases, he says, surgery can successfully prevent new strokes in his young patients.
“We have the potential,” he says, “to turn around patients’ lives.”
FOR INFORMATION: 410-955-7337

