
The outlook for many patients diagnosed with breast cancer has improved in recent years. Through molecular profiling and other technologies, researchers have found ways to better characterize tumors and tailor treatments to the unique tumor signature as well as the overall health of each patient. No longer are there “one size fits all” treatment solutions. Your treatment team will discuss with you care strategies that might include surgery, chemotherapy, immunotherapy, targeted therapies as well as radiation and radiosurgery.
Radiation is a powerful tool in the treatment of breast cancer. It is often used in combination with surgery as well as when surgery is not an option. It is also used to re-treat areas of previous disease.
Why Radiation Therapy?
Radiation therapy kills cancer cells using high-energy x-rays or particles. The most common approach for breast cancer radiation involves post-operative therapy, delivered after surgery to prevent a tumor from returning in the treated area.
Our radiation oncologists most commonly use a type of photon-based external beam radiation called three-dimensional (3-D) conformal radiation therapy. For this technique, imaging scans are used to create a three-dimensional model of the exact shape and size of the radiation target. Then multiple radiation beams are aimed at the target area, sparing nearby healthy tissue.
In some cases, other techniques, such as intensity-modulated radiation therapy (IMRT), may be used. IMRT delivers targeted radiation doses to the tumor site, patterned to match the shape of the tumor through modulating the intensity of the radiation beams.
By using computed tomography (CT) simulation during treatment planning, the oncologist can place the patient in the ideal position for radiation delivery. This also allows the oncologist to distribute an even radiation dose over the breast and other target areas, ensuring sufficient delivery to these areas while minimizing side effects.
Patients may be treated in either the prone (face down) or supine (face up) positions, depending on the clinical scenario and the patient’s anatomy. In some cases, a prone breast board can improve the evenness of the radiation dose and protect the patient’s heart and lungs.
When needed, we recommend specific breath-hold techniques for patients with left-sided breast cancer who are being treated in the supine position. These techniques are known to protect the heart during radiation.
Proton Therapy for Breast Cancer
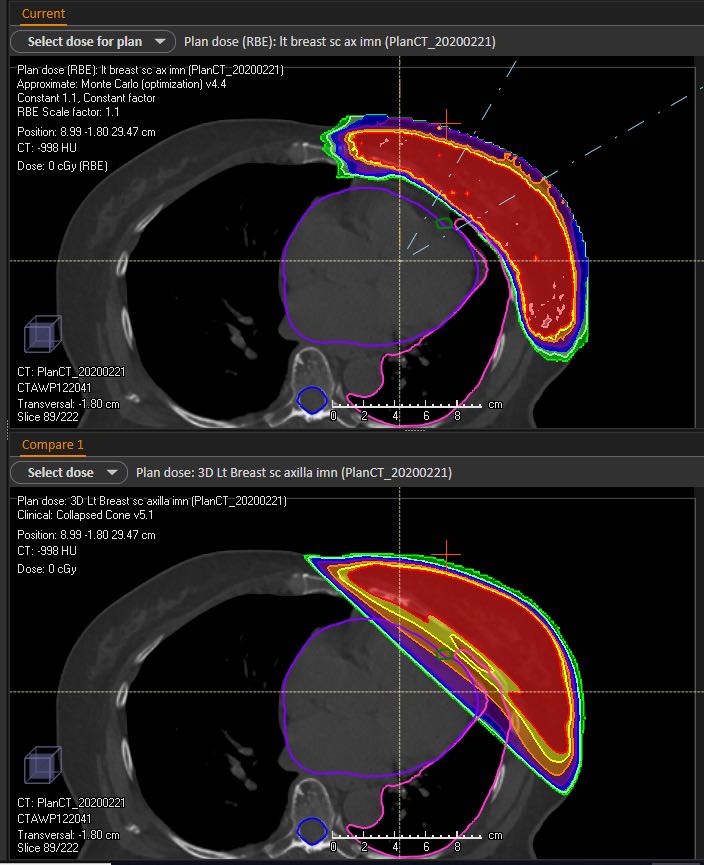
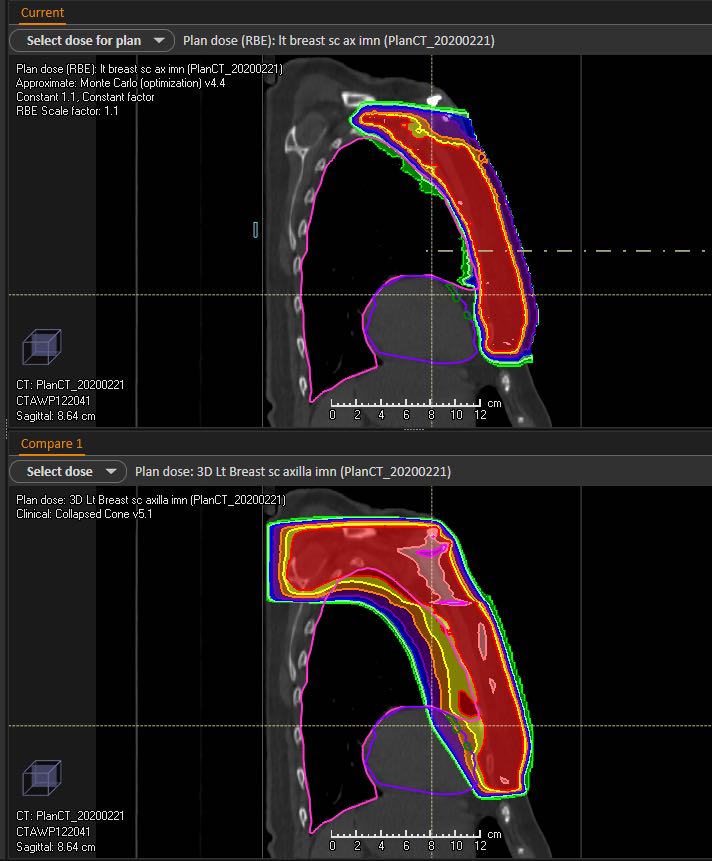
Proton therapy is a unique type of external beam treatment. It takes advantage of how protons deposit radiation dose as they move through the body. Unlike photon therapy that uses X-ray beams, which do not stop as they pass through the body, the depth of proton therapy beams can be more precisely controlled. As the protons come to a stop, all of their energy is deposited within the target with little to no exit dose past the target to the surrounding tissues.
With image guidance and pencil beam scanning technology, proton therapy at the Johns Hopkins Proton Center is among the most advanced in the world. Pencil beam technology allows for “dose painting” with a precise proton beam only a few millimeters wide to target the unique shape of individual targets.
Proton therapy may hold advantages for patients withbreast cancer, particularly those with cancers that require treatment of the internal mammary lymph nodes. Because of their proximity to the heart, treating these lymph nodeswith proton therapy instead of photon therapy could significantly reduce radiation exposure to the heart, potentially reducing the risk of subsequent cardiac disease later in life. This question is actively being stidued in a nationwide randomized clinical trial called the Radiotherapy Comparative Effectiveness (RADCOMP) Study, which is open at our Johns Hopkins sites. Eligible participants include those who need radiation to the intermal mammary lymph nodesand have no evidence of cancer spread to other parts of the body.
Many factors are taken into consideration when discussing breast cancer treatment with proton therapy. These include:
- Patients with pre-existing cardiac or lung conditions
- Patients with left sided breast cancer who need the internal mammary lymph nodes treated
- Prior radiation therapy in the same area
- Unique considerations regarding the patient’s anatomy
Our team assesses each patient individually and develops a tailored treatment recommendation, which may include protons in selected cases. Patients who need their internal mammary lymph nodes treated may be considered for enrollment on the randomized clinical trial, RADCOMP.
Proton Therapy Breast Cancer Experts:
Sara Alcorn, MD, MPH, PHD
Victoria Croog, MD
Marie Kate Gurka, MD

